What is “cancer screening”?
Screening for any cancer envisages specific examination of people who don’t have any symptoms (asymptomatic), but belong to an age-specific cancer risk group. The purpose of any cancer screening is to detect the disease at an early stage, thereby reducing the mortality rate associated with that specific cancer, as well as to assess the risk of developing this specific cancer in case no symptoms are manifested. Screening can contribute to early detection of cancer, resulting in a higher chance of curability. Efficiently organized screening programs require availability of sufficient resources for screening, as well as appropriate diagnostic work-up for abnormal lesions followed by a timely, accessible, and effective treatment and management of the diagnosed disease.
The internationally accepted methods of cancer screening programs are population-based/organized (defined target population) and opportunistic (when/where appropriate).
Population-based screening programs
Organized programs are characterized by centralized screening invitations to a well-defined target population, systematic call and recall for screening, delivery of test results, investigations, treatment and follow-up care, centralized quality assurance, and a program database with linkages to other information systems, such as cancer registration systems and death registration systems, for monitoring and evaluation of the program. The screening policy of an organized program defines at least the screening protocol, the repeat interval, and the determinants of eligibility for screening. Effective communications should also be supported enabling the target population to make an informed decision about whether to participate. In addition, organized programs include an administrative structure, which is responsible for service delivery, including follow-up of detected lesions, quality assurance, and evaluation.
Opportunistic screening programs
Opportunistic programs are not tailored to a predetermined eligible population and provide screening tests on request or at the time of routine health examinations. These programs are less amenable to quality assurance than population-based screening, due, among other things, to the lack of administrative and organization infrastructure. They rely on the initiative of individual healthcare providers to offer screening or to encourage participation in a screening program or outside the context of any program (so-called “wild” screening).
Current cancer screening programs in Armenia
Cervical cancer screening program
Cervical cancer is the only type of cancer that can be prevented and treated. It develops during a period of about 10-20 years. If we have women dying from this disease in nowadays Armenia, it is the drawback of the country’s healthcare system in general, as well as the indifferent attitude of women towards their own health. Armenian women, taking up the comprehensive care of the family, usually neglect their own health and consult a doctor when the intervention may be too late. In 2015 a population-based cervical cancer screening program was launched throughout Armenia, using PAP smear test. Participation in the screening program is free for a target population group, please consult your primary healthcare staff if you meet the screening requirements.
Cervical cancer screening program 2.5MB (pdf)By the Order No.1984-A of the Minister of Health of the Republic of Armenia dated July 22, 2019 a national Board was established to coordinate the improvement and efficiency management of cancer care in Armenia.
The Order also approves the structure and operations of the national Board. Among 18 members of the Board, HENARAN charitable foundation, as a cancer patient advocacy organization in Armenia, is the only non-governmental organization to represent the voice and interests of cancer patients.
Since its inception in July 2019 the Board worked to draft the working document for the “Strategy for combatting malignant neoplasms 2019-2023” and its justification.
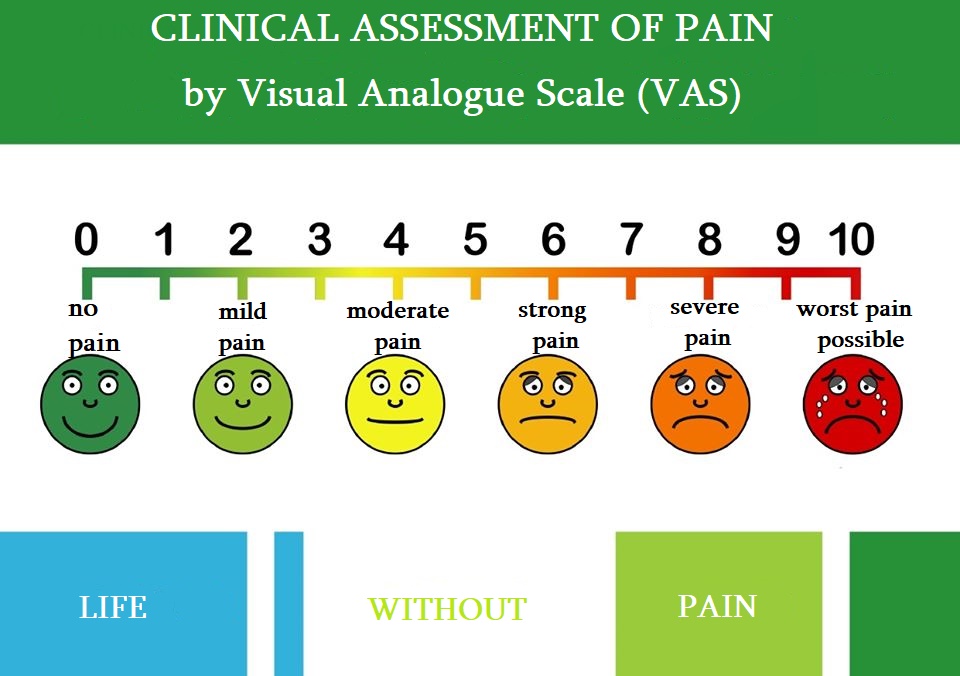
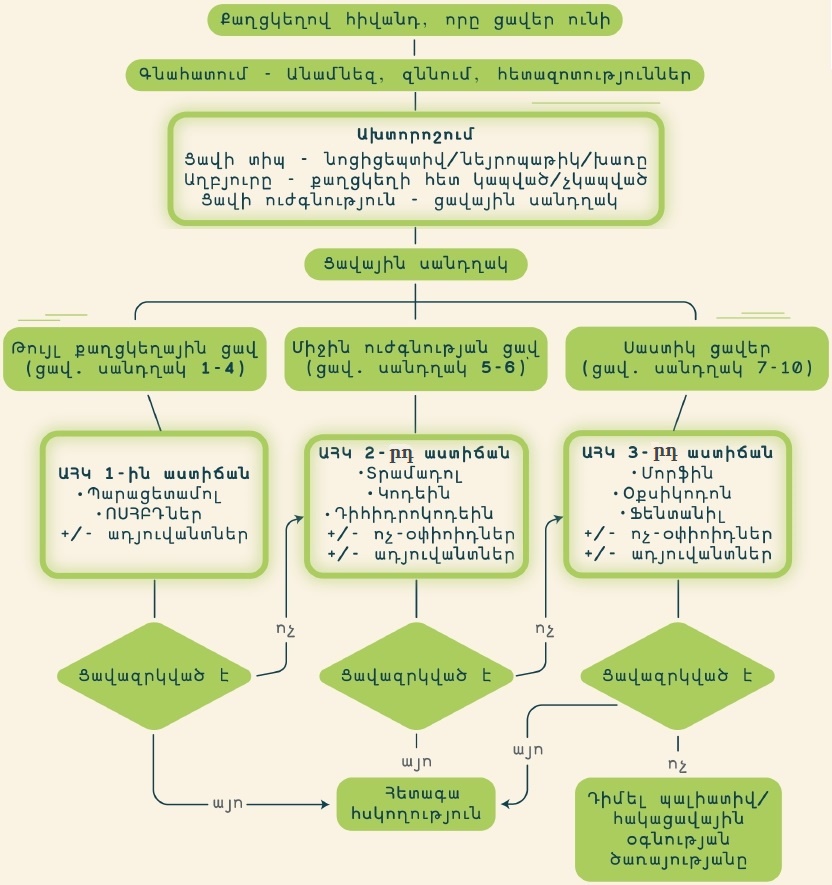
Effective analgesia is accessible if appropriate analgesics of the appropriate size and quantity are prescribed. Despite many problems, especially in the provinces and rural areas, together we can improve the accessibility of palliative care in Armenia when patients are empowered and protect their rights.
Unfortunately, most problems occur due to prescription or provision of strong painkillers of the inappropriate type, size, or quantity. Doctors avoid prescribing opioids for pain relief. Patients or their relatives most often mention that doctors do not prescribe morphine or other strong painkillers, saying, "There will be a heart attack", "Do you want us to be sued?", “We are not allowed to do that, it is the last resort” and other similar expressions. We urge doctors to strictly follow the established order and clinical guidelines for provision of narcotics and psychotropic substances that are approved by the orders of the RA Ministry of Health, to be guided exclusively by legal acts and not yield to stereotypes.
The framework of legal acts and clinical expertise for provision of palliative care in Armenia includes:
1. Criteria for provision of palliative care (RA Minister of Health Order No.45-N dated October 18, 2017)
2. Clinical guidelines for prescribing narcotics and psychotropic substances for management of the pain syndrome (RA Minister of Health Order No.2910-A dated December 11, 2014)
3. Clinical guidelines on assessment and management of the patient’s pain (RA Minister of Health Order No.751-A dated March 22, 2018 )
4. Guidelines on arrangement of activities of doctors and nurses (RA Minister of Health Order No.2911-A dated December 11, 2014 ) and others.

It is difficult to reconcile oneself to the diagnosis of cancer and this becomes a serious problem for many patients and their families.
HENARAN Foundation can help you better understand the cancer-related issues, treatment options and support activities, as well as set up through a “support group” useful communication with other patients, including cancer survivors. HENARAN Foundation will help you understand how to navigate through healthcare system, give a briefing on your patient rights, as well as provide contact information of consultants, home care service providers, education and information centers.
No person and family should be left alone in the fight against cancer. There are several non-governmental resources available in Armenia that could assist you and your family in different ways.

Cancer.am information portal
Follow us on Facebook
Website

Armenian Psycho-Oncology Association
Follow us on Facebook
Website

Bridge of Health-Armenia charitable foundation
Follow us on Facebook
Website

Fund 100 charitable foundation
Follow us on Facebook
Website

Menq Enq charitable foundation
Follow us on Facebook

City of Smile charitable foundation
Follow us on Facebook
Website

OGNEM foundation
Follow us on Facebook
Website

Europa Donna Armenia NGO
Follow us on Facebook

Ani Haykuni Cancer Treatment Support foundation
Follow us on Facebook
Website

“Hand in hand” health protection Armenian association NGO (Ijevan, Tavush)
Follow us on Facebook

Center for Rights Development NGO
Follow us on Facebook

“Life without pain” movement for access to palliative care
Follow us on Facebook
The 9th WE CAN Eastern Europe and Central Asia Advocacy Summit on Breast and Cervical Cancer was held in Yerevan, Armenia, on October 11-12, 2019.

The international Summit was attended by 30 advocates from Armenia and another 25 advocates from 12 countries of the Eastern Europe and Central Asia. The US Ambassador Lynn Tracey and the RA Deputy Minister of Health Anahit Avanesyan delivered welcome speeches emphasizing the importance of the Summit. The very intensive programme of the two-day Summit allowed the participants to further enrich their knowledge base, network and establish new connections and form partnerships.
The Summit was initiated by the Women’s Empowerment Cancer Advocacy Network (WE CAN – Women’s Empowerment Cancer Advocacy Network, www.womenscanceradvocacy.net). HENARAN charitable foundation was the national hosting organization in Armenia, while the summit took place at the Armenian-American Health Center at no cost and with great service and reception.
Within the framework of the Summit the Armenian Cancer Patient Advocates Alliance (ACPAA) was formed, and its members – cancer patient advocates - presenting themselves as civil society organizations of the Republic of Armenia, individuals, and cancer patients and survivors, declared their commitment to join efforts to prevent cancer and provide cancer patients with personalized support, ensure access to cancer treatment and care, strive for exercise and protection of healthcare and social rights.

The Armenian Cancer Patient Advocates Alliance formed within the framework of the Summit authored a DECLARATION, with a call on specific actions and measures addressed to the RA Government, the RA Ministry of Health, the RA National Assembly, Yerevan State Medical University, state and non-state stakeholder organizations. The Declaration received a great response among the civil society and state authorities, whereby shortly after its publication authorized entities took specific measures to address some problems outlined in the Declaration, which will be a continuous process.